Take the Ultimate Circulatory System Practice Test!
Ready to master blood flow and immune defense? Start this blood circulation quiz now!
Ready to test your expertise with a dynamic circulatory system practice test? Dive into our free circulatory system quiz, covering everything from blood flow and vessel dynamics to heart health and immunity. You'll tackle a fun blood circulation quiz and explore key defense mechanisms with immune defense trivia, and even take our cardiovascular system quiz for advanced rounds. Perfect for students, educators, and science enthusiasts, this challenge doubles as a cardiovascular system practice test that highlights real-world applications in medicine and wellness. Boost your confidence, identify learning gaps, and elevate your scores in minutes - begin now!
Study Outcomes
- Understand Circulatory System Components -
Identify the anatomy and function of the heart, blood vessels, and blood as the primary components of the circulatory system.
- Trace Blood Flow Pathways -
Map the route blood takes through the heart chambers, pulmonary circuit, and systemic circulation to appreciate how oxygen and nutrients reach tissues.
- Analyze Blood Composition and Function -
Examine the roles of red blood cells, plasma, and platelets in transporting gases, nutrients, and clotting factors throughout the body.
- Describe Immune Defense Mechanisms -
Differentiate between innate and adaptive immune responses, including how white blood cells and antibodies protect against pathogens.
- Evaluate Cardiovascular Health Factors -
Assess common risk factors and conditions that affect heart health, such as hypertension and atherosclerosis, through scenario-based questions.
- Apply Knowledge in Practice Questions -
Use your understanding to tackle circulatory system practice test items, reinforce learning, and boost confidence in blood circulation quiz and immune system practice test topics.
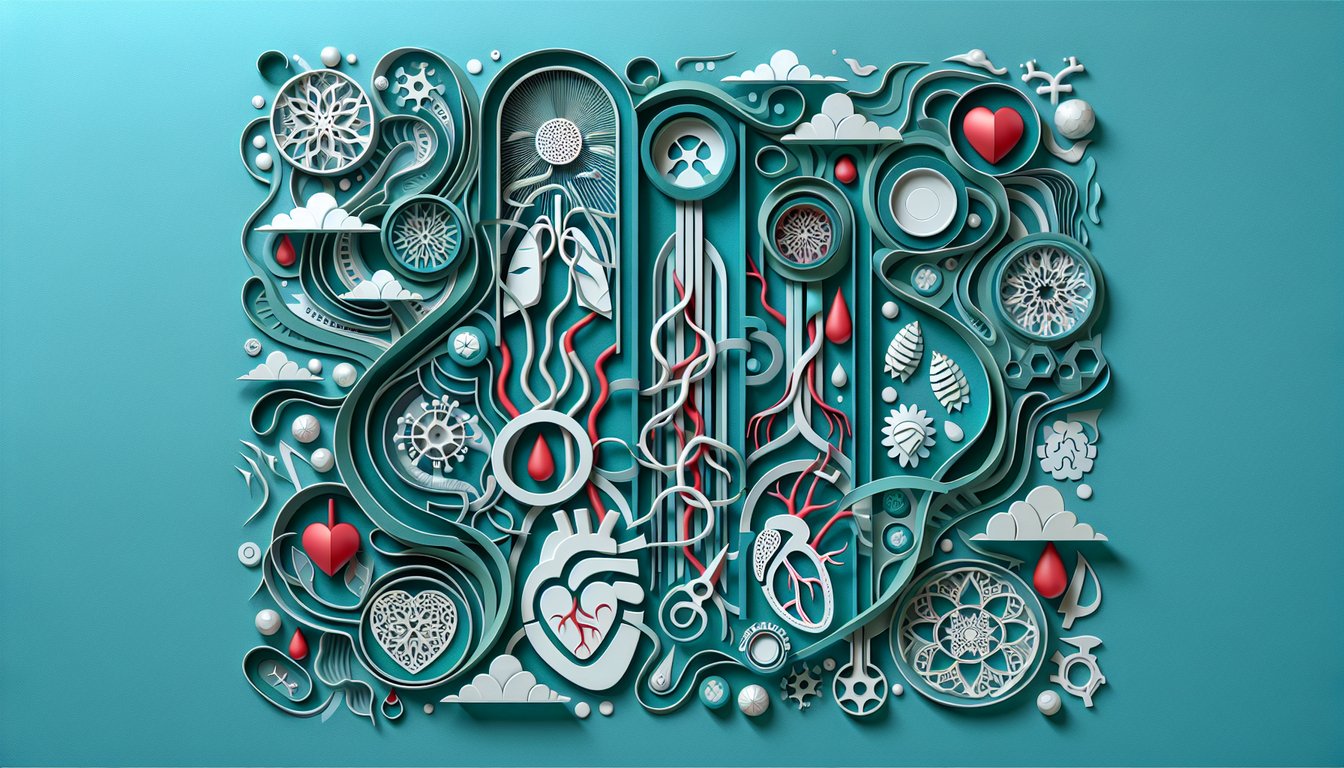
Cheat Sheet
- Systemic and Pulmonary Circuits -
Review the flow from the right atrium through the pulmonary circuit and back into the left ventricle, then out via the systemic arteries. A handy mnemonic is "RA-RV-PA-LA-LV-Aorta" to recall the path. According to the American Heart Association, mastering this route is essential for any circulatory system practice test.
- Cardiac Output and Blood Pressure Formulas -
Use the formula CO = HR × SV (cardiac output equals heart rate times stroke volume) to calculate how much blood the heart pumps per minute. Combine this with MAP = CO × TPR (mean arterial pressure equals cardiac output times total peripheral resistance) for blood pressure regulation questions. These equations appear frequently in Harvard Medical School physiology outlines.
- Blood Components and Functions -
Understand that plasma carries nutrients and hormones, red blood cells transport oxygen via hemoglobin, and white blood cells drive immune defense. A quick fact: adult hematocrit is roughly 45%, with hemoglobin at 13 - 17 g/dL in men and 12 - 15 g/dL in women (NIH data). Expect these figures on any blood and circulatory system quiz.
- Innate vs. Adaptive Immunity -
Differentiate innate barriers like neutrophils and macrophages from adaptive players such as B-cells and T-cells. Mnemonic: "M&M" for Macrophages (innate) then Memory B-cells (adaptive) to track first response and long-term immunity per CDC guidelines. This concept is key on immune system practice tests and blood circulation quizzes alike.
- ABO and Rh Blood Group Compatibility -
Memorize that type O is the universal donor ("Oh yes, I can give to all!") and AB is the universal recipient (All Be Received). The American Red Cross compatibility chart ensures you know which transfusion pairs are safe. Transfusion compatibility shows up often on cardiovascular system practice tests.