Bone Cell Practice Quiz: Test Your Knowledge
Sharpen cell biology skills with interactive questions
Study Outcomes
- Identify and describe the structure and function of key bone cells.
- Analyze the differences between various bone cell types.
- Understand the role of bone cells in bone growth and remodeling.
- Apply knowledge of bone cell mechanisms to solve biology problems.
Bone Cell Quiz: Exam Review Cheat Sheet
- Osteoblasts - These enthusiastic builders are the bone equivalent of bricklayers, secreting collagen and triggering mineral deposits that harden into sturdy bone. Without them, our skeleton wouldn't have the strength to support daily adventures or heal after a break. Learn more
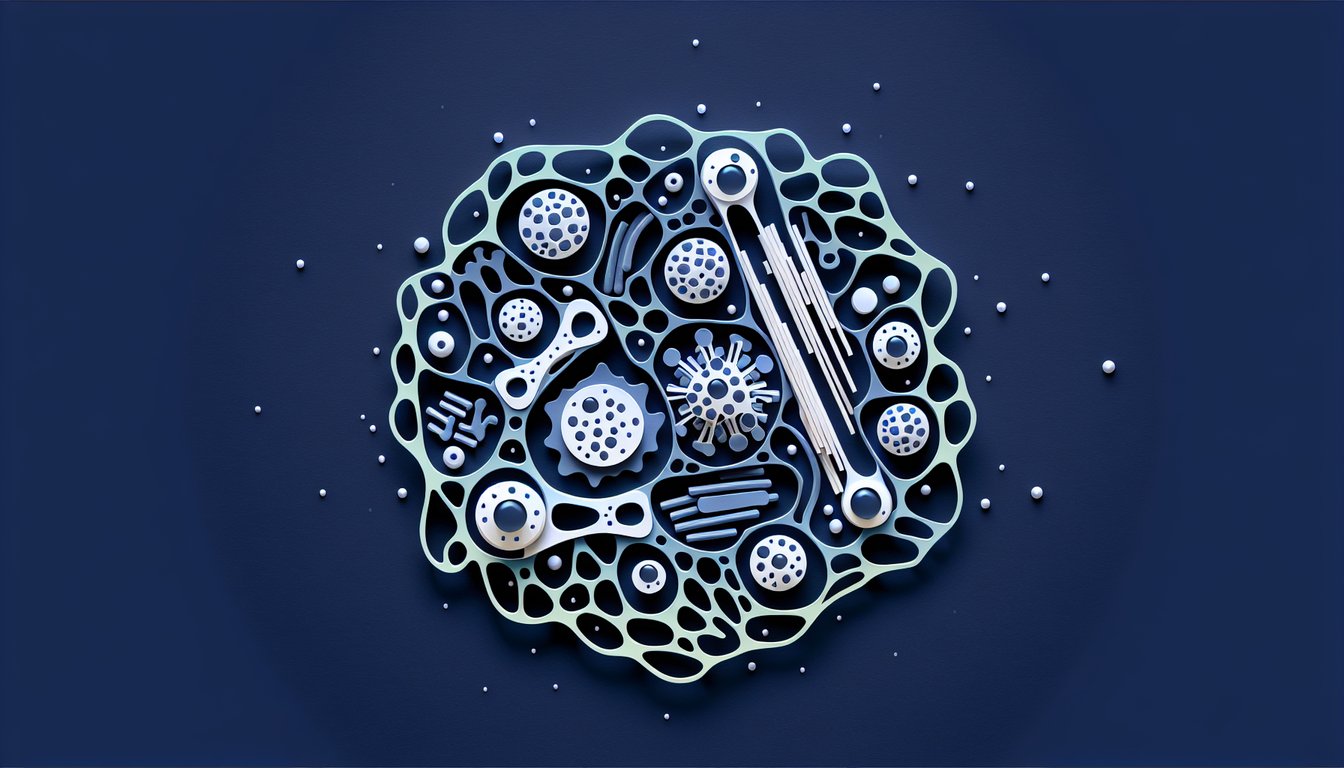
- Osteocytes - Once osteoblasts get trapped inside the bone matrix, they transform into osteocytes, the resident "sensors" that monitor mechanical stress and direct remodeling crews where strength is needed most. Their long, spider-like arms form a communication network essential for bone maintenance. Learn more
- Osteoclasts - These large, multinucleated powerhouses break down old bone by secreting acids and enzymes, releasing stored minerals into the bloodstream. They help maintain calcium balance and pave the way for new bone formation. Teamwork between osteoclasts and osteoblasts keeps bones healthy and adaptable. Learn more
- Bone Lining Cells - These flat, resting osteoblasts cover inactive bone surfaces, controlling the traffic of calcium and phosphate. They can spring into action as osteoblasts when repair is needed, like cells on standby. Their vigilance helps maintain bone homeostasis around the clock. Learn more
- Bone Matrix - Think of the bone matrix as a biological composite: flexible collagen fibers give it a bit of bend, while rigid hydroxyapatite crystals provide rock-solid strength. This perfect combo lets bones absorb impacts without snapping. It's a marvel of natural engineering that balances toughness and resilience. Learn more
- Bone Remodeling - Bones aren't static - they're in a continuous cycle where osteoclasts remove old or damaged tissue and osteoblasts fill in the gaps with fresh bone. This dynamic process adapts our skeleton to new stresses, repairs micro-damage, and helps regulate calcium levels. It's how bones stay strong through every stage of life. Learn more
- Calcium Homeostasis - Bones act as the body's main calcium vault, releasing Ca²❺ when levels drop and storing excess when levels rise. Osteoclasts withdraw calcium into the blood, while osteoblasts lock it back into the matrix. This tug‑of‑war is vital for muscle contraction, nerve impulses, and more. Learn more
- Mechanical Stress - Ever heard "use it or lose it"? Osteocytes sense mechanical loads - like running, jumping, or even dancing - and signal osteoblasts and osteoclasts to reinforce or reshape bone accordingly. Regular activity keeps your skeleton strong and responsive to everyday demands. Learn more
- Hormonal Regulation - Hormones like estrogen, calcitonin, and parathyroid hormone choreograph the bone remodeling dance, tweaking osteoblast and osteoclast activity. These chemical messengers influence peak bone mass, maintenance during adulthood, and bone loss in later years. Understanding them is key to managing bone health across the lifespan. Learn more
- Bone Diseases - When the balance between bone resorption and formation tips too far - often due to hormonal shifts or aging - conditions like osteoporosis can arise, leaving bones weak and prone to fractures. Studying how each cell type contributes to remodeling helps us develop prevention strategies and therapies. Keep your bones battle-ready! Learn more